Adrienne A. Boire, MD, PhD
When cancer cells escape their primary tumor and move to the fluid and tissues surrounding the brain and spinal cord, the result is devastating. This difficult to treat condition, called leptomeningeal metastasis, may cause pain, seizures, difficulty thinking, and a loss of muscle, bowel, and bladder control. Now, Damon Runyon Clinical Investigator Adrienne A. Boire, MD, PhD, and colleagues at Memorial Sloan Kettering have discovered how these rogue cells are able to survive in the barren environment of the cerebral spinal fluid (CSF) and suggest a possible strategy for treatment.
The researchers found that cancer cells reprogram themselves to absorb iron as a way to thrive and grow while other cells — notably immune cells that reside in the same space — are left short.
To investigate how cancer cells survive in CSF, the researchers analyzed fluid samples taken from five patients with leptomeningeal metastasis and conducted a test called single cell RNA sequencing of the cancer cells in the fluid.
The analysis revealed that the cancer cells increase their activity of a gene called Lipocalin-2, which produces a protein that binds iron. The cancer cells can boost their production of the Lipocalin-2 protein levels to outcompete the immune cells for iron in the surroundings.
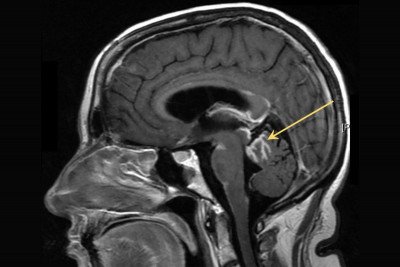
indicated by the yellow arrow) occur
when cancer cells from a primary tumor
spread to the fluid and tissues lining
the brain and spinal cord.
“It’s nefarious, the way the cancer cells exploit Lipocalin-2 to gain an advantage over the immune cells,” Dr. Boire explains. The immune cells in the CSF lack the ability to attract more iron and suffer as a result. This raises intriguing questions about why immune cells may behave differently around the brain and spinal cord. Normally, immune cells can produce the needed protein and compete for iron, so something is disabling them. “If we find out, we could possibly help patients with central nervous system cancers benefit from immune therapies, which often don’t work in the nervous system for reasons we don’t understand,” Dr. Boire says.
The researchers then tested what effect cutting off access to iron would have on the cancer cells. In mouse models for the disease, they delivered chemical compounds called iron chelators that bind iron directly into the spinal fluid. As they hoped, growth of the cancer cells slowed down without iron available.
The researchers are working to bring this therapy to a clinical trial. They think the treatment will be safe if the chelators are confined to the CSF. “When cancer gets in the CSF, it is sealed away in its own ecosystem, which is why it’s hard to treat. But if you can deliver drugs into that space, the treatments don’t go anywhere else, so side effects are limited.”
Read more: Memorial Sloan Kettering News
Original research published in Science.